A new model of care could save lives and money in the fight against hypertension. These are the findings of new analysis done by Broadstreet and research partners Ross Tsuyuki at the University of Alberta, and Carlo Marra, University of Otago on behalf of the Canadian Pharmacists Association. High blood pressure is a key risk factor for cardiovascular disease, kidney failure and death and affects about a quarter of the planet’s population.1 It also accounts for around 10% of direct medical costs globally.2 In Canada, around 5.3 million people have high blood pressure3 and particularly concerning is the fact that a third of all cases are not adequately controlled.4,5
That lack of adequate control lies at the heart of this new research. Enabling people to bring their blood pressure under control could significantly increase quality of life, as well as prevent cardiovascular issues, kidney failure and even death. The study looks at the health benefits and economic impacts of a new model of care, one which increases the level of pharmacist intervention in the management of a patient’s hypertension. When a pharmacist is using the full scope interventions available to them this could include assessment of and counselling about cardiovascular risk and blood pressure control, reviewing antihypertensive medications, prescribing/titrating of drug therapy, laboratory testing, and follow up visits with the patient.
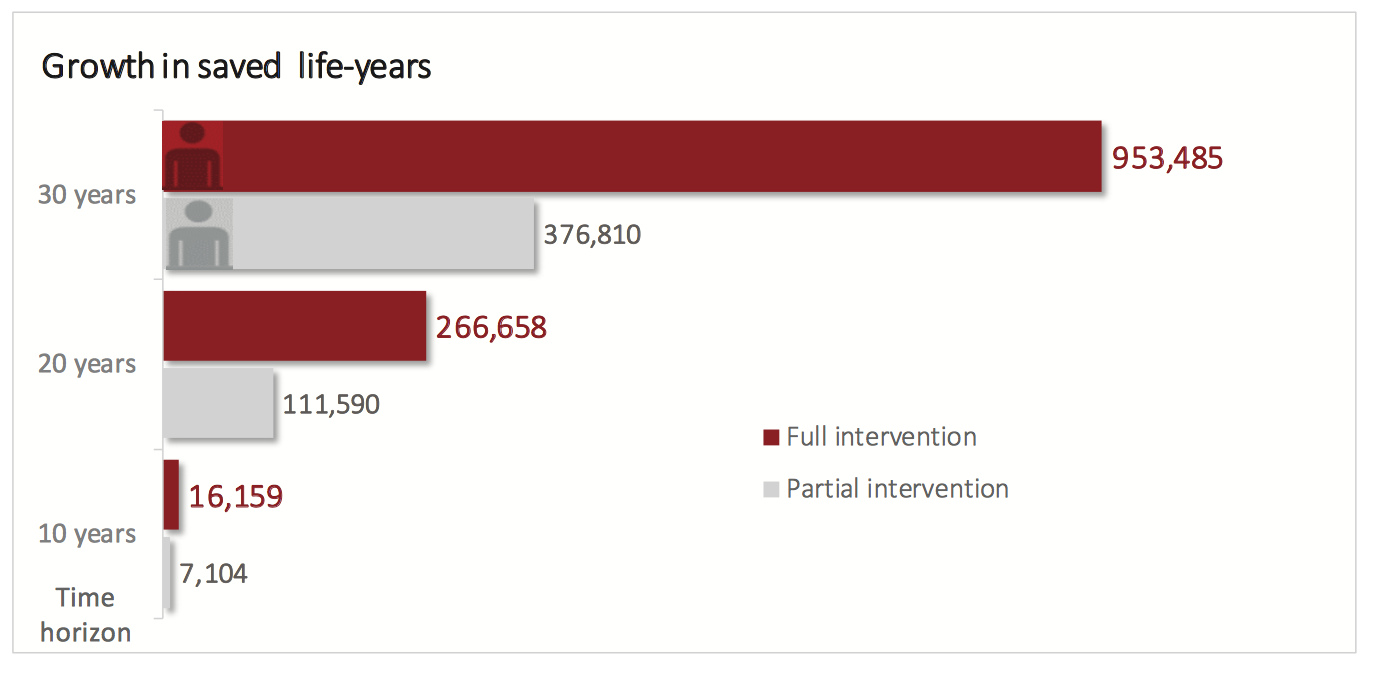
Starting with a base case of 30 years, the study developed a model that can be adjusted for different levels of pharmacist intervention, health outcomes and time frames. The model shows that for the country as a whole, over 30 years, full scope pharmacist intervention (which previous research has shown can achieve an average 18.3mmHg reduction in systolic blood pressure6) would see 130,000 fewer strokes; 260,000 fewer myocardial infarctions; 76,000 fewer cases of angina; 70,000 fewer instances of heart failure; and 1,800 fewer instances of kidney failure. And the benefits are not just to health, by preventing the sorts of serious medical consequences resulting from high blood pressure, the analysis shows the intervention would result in savings of around 15.7 billion dollars on a national level, even when factoring in cost related to increased visits to pharmacists.
At Broadstreet, a key part of what we do is using cutting edge IT solutions to ensure that important findings have the maximum impact. We believe the results of this project are vitally important to Canadians. Because of that, we have created an interactive tool that tells the story of the analysis. It lets you explore the research model and demonstrates visually how hypertension health and economic outcomes would change with different levels of pharmacist intervention and over different timeframes. Check it out on the website of the Canadian Pharmacists Association.
Listen to Broadstreet Principal Karissa Johnston explain the study and its potential impact to CBC Early Edition’s Rick Cluff. (40:30)
- Collaboration NCDRF. Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389(10064):37-55.
- Gaziano TA, Bitton A, Anand S, Weinstein MC, International Society of H. The global cost of nonoptimal blood pressure. J Hypertens. 2009;27(7):1472-1477.
- StatCan. High blood pressure, by sex, and by province and territory 2014; http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/health70a-eng.htm, 2017.
- Canada. S. Blood pressure of adults, 2012 to 2015. Health Fact Sheets 2016; http://www.statcan.gc.ca/pub/82-625-x/2016001/article/14657-eng.htm, 2017.
- Padwal RS, Bienek A, McAlister FA, Campbell NR, Outcomes Research Task Force of the Canadian Hypertension Education P. Epidemiology of Hypertension in Canada: An Update. Can J Cardiol. 2016;32(5):687-694.
- Tsuyuki RT, Houle SK, Charrois TL, et al. Randomized Trial of the Effect of Pharmacist Prescribing on Improving Blood Pressure in the Community: The Alberta Clinical Trial in Optimizing Hypertension (RxACTION). Circulation. 2015;132(2):93-100.
