Asthma affects more than 4 million Canadians, making it the third most common chronic condition in the country.(Government of Canada 2024) Between 5-10% of those 4 million+ have severe asthma.(Chung, Wenzel et al. 2014) For these individuals, achieving control of their asthma is difficult, even when following a strict regimen with multiple medications and managing their asthma triggers and co-occurring conditions. For those living with severe asthma, the impact on their quality-of-life is substantial and detrimental. Day to day, patients experience fear, anxiety, and frustration about their symptoms and the potential risk of hospitalization if the symptoms are exacerbated.
Exacerbations are often treated with oral corticosteroids (OCS), but these can be accompanied by distressing side effects. The introduction of biologic therapies in the early 2000s marked an important change in the treatment landscape for severe asthma. As an add-on treatment, biologics offered significant clinical and quality-of-life benefits including reducing symptoms, asthma exacerbations, and corticosteroid use. However, they are not suitable for all individuals with severe asthma. Data from clinical trials and other sources has helped us understand the clinical and safety benefits of biologics, but to date, information on patient perspectives on these treatments has been limited. In order to address this knowledge gap, Broadstreet and Asthma Canada have worked together on a study that sought to understand the preferences and priorities of Canadians with severe asthma with regard to biologic therapies, the results of which were recently published in Advances in Therapy.
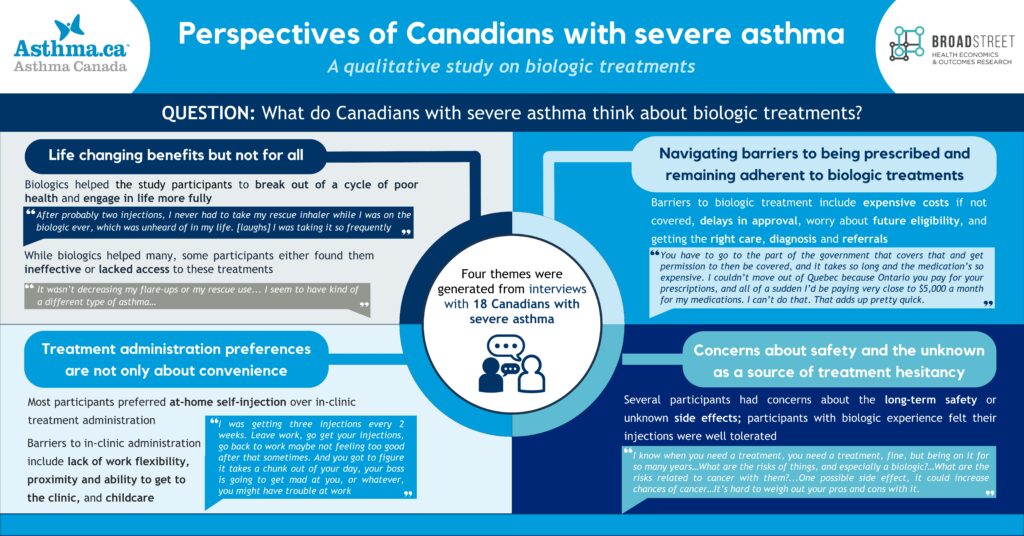
The study involved conducting semi-structured interviews with Canadians with severe asthma, some of whom had prior experience with biologics. In the interviews, the participants described their daily life with severe asthma, their experiences and priorities related to asthma treatment, and their impressions of biologics ─ either through their own experience or their perceptions based on what they knew about biologics. Once the interviews were complete, the study team used reflexive thematic analysis to explore patterns in the data.
Among the 18 participants, 10 were currently taking or had prior experience with biologics for asthma, four were unfamiliar with them, two were considering treatment with biologics, and two believed that they may not be eligible.
Participants described health problems they experienced related to severe asthma, including asthma attacks leading to hospitalization; prolonged, severe, and unpredictable bouts of illness; struggling with daily symptoms; side effects from treatment with OCS and antibiotics; and the compounding effect of comorbidities. Physical health problems also impact social and emotional well-being. Emotional impacts included feelings of sadness, guilt, frustration, anxiety, and stress; and many participants noted a lack of understanding from others. Moreover, participants recounted challenges getting the treatment and health care services they needed.
The above-noted challenges experienced by participants in turn shaped their overarching treatment priorities, and participants emphasized the importance of good asthma control for improving their well-being.
The researchers generated four main themes from the interview data related to perceptions of biologics for severe asthma:
- Biologics could offer life-changing benefits, but not for everyone.
- People with severe asthma must navigate financial and healthcare system barriers to be prescribed and remain on biologic treatments
- Participants expressed preferences related to treatment administration that were about more than convenience.
- People with severe asthma have concerns about safety and the unknown which were a source of treatment hesitancy.
The findings of our study suggest that the clinical benefits of biologics align with patient perceptions of achieving good asthma control. However, treatment gaps persist among individuals who do not experience a meaningful improvement in their asthma symptoms and those who face barriers to accessing biologics. People with severe asthma placed more importance on greater availability of at-home treatment options, improved access to financial support to cover treatment costs, and support to address safety concerns.
We believe this research plays an important role in providing insight into patient-based treatment priorities and preferences for biologics, which may help inform decision-making related to emerging therapies for severe asthma.
If you are interested in qualitative methods to address some of your research objectives, either as a stand-alone or as a precursor to quantitative work like a discrete choice experiment, Broadstreet has the expertise and experience to help. Get in touch to discuss how we can work together to achieve your research goals.
Chung, K. F., et al. (2014). “International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma.” European Respiratory Journal 43(2): 343-373.
Government of Canada (2024). “Canadian Chronic Disease Surveillance System (CCDSS) 2023 Data Tool: Trend Over Time.” Retrieved June 28, 2024, from https://health-infobase.canada.ca/ccdss/data-tool.
Please contact the authors if you would like a copy of the paper.

